Opinion: Mental Illness Is Not a Crime, So Let’s Stop Treating It Like One
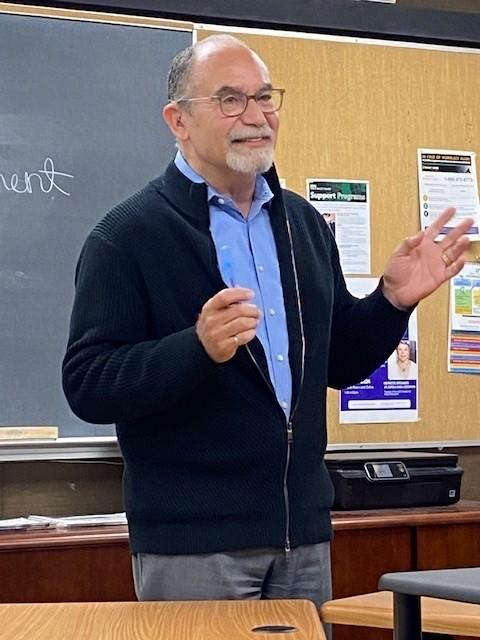
A fellow student in one of my classes suffered a mental health episode recently, and campus police were called to intervene. The situation was extremely difficult to watch as the actions of the police seemed to further distress the student, who was lying on the ground, curled up and screaming.
Officers hovered over the student, attempting to escort them out of the classroom as their screams of agony grew louder. The student was clearly resisting, and it seemed that no one, not even the police officers who were called in to deal with the situation, knew what to do.
I’m not writing this to shame the police officers. I know they followed protocol, and their job presents a range of challenges on a daily basis. But when it comes to mental health crises like the one my classmates and I witnessed, a traditional policing response isn’t always appropriate.
The intersection between mental health and law enforcement has become increasingly visible in recent years. According to the Washington Post, police fatally shot more than 1,000 people in the past year, and in 2015, “nearly a quarter of all people killed by police had a known mental disorder.”
Walter Wallace Jr., Ricardo Muñoz, and Angelo Quinto were all experiencing mental health episodes when they were killed by police officers, within months of each other in 2020, after their families called 911 requesting help. Too many mental health crises have ended in the same unfortunate outcome.
Police officers are the ones we count on to save us when we’re in danger. But it’s become difficult to ignore their misconduct, especially when it includes the deaths and assaults of non-criminal people who required more nuanced, delicate care.
Individuals experiencing mental health crises are often in a state of heightened emotional distress and may react negatively to the presence of police officers. This can lead to confrontational situations among individuals who feel threatened and police officers who feel they need to use force to control the situation.
Mental health crises require a compassionate and empathetic response that considers the root causes of the problem and provides appropriate support and treatment. Maybe things in the classroom would have been different that day if a mental health specialist had responded first instead of police.
On a local level, police departments say they have been striving to create reforms.
“Many academies now have blocks dedicated to mental health training which had been implemented sometime in the last 20 years,” said DVC Police Lieutenant Kathryn McDonald, who is a member of the Pleasant Hill Police Department in addition to her role as head of campus safety.
“After the academy, graduates are partnered with a training officer and have more training within their department,” she added.
Police training has been a central part of efforts to improve law enforcement’s response to people with mental illness. However, according to McDonald, “it’s nothing compared to the years of extensive training mental health specialists receive.”
While law enforcement officers may get some basic training in de-escalation techniques, they’re not necessarily equipped to provide the level of support that someone in a mental health crisis needs — and this is where collaboration between police and mental health professionals is crucial.
By working together, police officers can ensure that a person in crisis is safely transported to a mental health facility where they can receive the appropriate care. One solution in recent years has been Crisis Response Teams, which are alternatives to law enforcement in situations dealing with mental health.
For example, the Street Crisis Response Team in San Francisco takes a community approach to dealing with people experiencing mental health and substance issues. The team is comprised of a paramedic, a clinician, and a peer specialist. Peer specialists have been through the same experiences as people in need; their presence helps establish a connection and builds trust.
Teams like this not only benefit those in need but also save cities time and money: the implementation of crisis teams allows police officers to receive fewer calls about mental health and reduces the number of interactions between law enforcement and those experiencing a crisis.
Kathleen Bennet, a mental health counselor and licensed clinical social worker at DVC, said it would be impossible for the college to implement something similar to crisis response teams, or send specialists to accompany police officers, given the current staff size of the mental health department.
“There’s just me and another person who is in charge of basic needs,” Bennet said. “We would need more. I’m the only one in the community college district.”
Mental health awareness may be more visible today, leading to improved results on campus. But the actions aren’t adding up when it comes to an appropriate law enforcement response to mental health crises. There should be more support when addressing people’s extreme needs to ensure that all parties remain safe.
“Overall, I think everyone can benefit from more training, and there’s always room for improvement,” Bennet added.
In the end, “mental health people should respond to mental health situations.”
(Illustration by Ericka Carranza)